CAPITATION OF PROFESSIONAL SERVICES: WHAT WE KNOW
Pacific Cardiovascular Associates Medical Group, Inc. (PCA) and Fresenius Medical Care North America (FMCNA) have a strategic partnership designed to grow and expand their current cardiovascular service scope and patient base, facilitate the broad adoption of PCA’s highly successful population management programs and together develop a cardio-renal strategy to better manage cardiac and renal patients and the underlying pathobiology of these chronic conditions.

As pioneers in embedding evidence-based best practices and performance improvements within capitated and other at-risk arrangements, PCA has established the standard for managing the cardiovascular care for large and diverse patient populations efficiently and cost effectively. PCA has been the purveyor of the value proposition for care coordination long before it became the narrative of the day.
PCA achieved this long-term vision by holding true to core practice fundamental principles, avoiding short-term thinking and misaligned short-term rewards. By investing in a sustainable future, PCA has significantly influenced the development of a premier model for cardiovascular care delivery.
Capitation Management Strategy
Capitation is a fixed amount of money paid to a provider in anticipation of the rendering of a service to a patient (member) who has selected the provider, or the limited network of contract providers, in advance of the need for the service. The money is usually paid monthly, and, while it may vary due to the age and gender of the patient, it is independent of the actual volume or cost of the services rendered. This payment is referred to as per member per month (PMPM) payment.
PCA’s strategy to manage the professional component of risk in delivering quality and affordable care is focused on maintaining stability, encouraging innovation, and reducing variability. As such, PCA may be viewed as an indispensable partner in caring for patients to those payors who buy cardiovascular disease care services. By pioneering value-based Accountable Care Organization (ACO) strategies, PCA manages cost by eliminating waste and inefficiencies, as well as assisting shared and global risk partners to get the right care for the right patient at the right time.
PCA delivers evidence-based, high-quality care for a diverse patient population and ensures consistent high performance by assessing patient and referring physician satisfaction and clinical performance. Technology and information infrastructure investments provide PCA with electronic medical record (EMR) and electronic practice management (EPM) systems, quarterly provider performance metrics, physician report cards, and performance-based incentive bonuses. PCA adopts a best practice standard and holds each provider accountable for their quality and outcomes.

By continually collecting data on patient care and provider performance, PCA is in a position to constantly monitor patient outcomes, population trending, and provider best practices. Standardization and guidelines ensure that patient care is delivered consistently throughout all markets for conditions like coronary artery disease, congestive heart failure, atrial fibrillation, and other structural or arrhythmia-related medical problems. In addition, rigorous auditing and review provide a constant near real-time feedback loop for the PCA medical staff. On the subject of value-based care, Dr. Toby Cosgrove of the Cleveland Clinic noted, “Data can help identify variations in clinical practice, utilization rates, and performance against internal and external benchmarks, leading to improved quality and a sustained change in culture.”2
Managing the capitation environment relies on effectively balancing patient-centered care with payor value expectations, physician and hospital partner perspectives, and political realities. PCA has established strategic relationships with large cardiovascular groups, hospitals, device and pharmaceutical companies, health delivery organizations, and payors.

Successes and Challenges in Capitation
PCA has consistently demonstrated high partner and stakeholder satisfaction in a large service market for a very diverse patient base—covering the geographic area in California from Torrance to San Diego—with established brand recognition. We continue to receive high quality ratings from independent health plan auditors. With demonstrable, excellent patient outcomes, PCA also has a low patient complaint rate and a high patient/ family word-of-mouth referral. We also are highly regarded by physicians and partner organizations.
The capitation market is a challenging environment, with medico- legal implications (Figure 1). Our primary challenges involve:
- Controlling costs
- Securing a large enough patient base with a favorable risk pool
- Realizing economies of scale
- Integrating vertically and horizontally across the care continuum
- Embracing population management principles
- Aligning incentives with partner delivery systems
Figure 1: Challenge Assumptions for Success
Conclusion
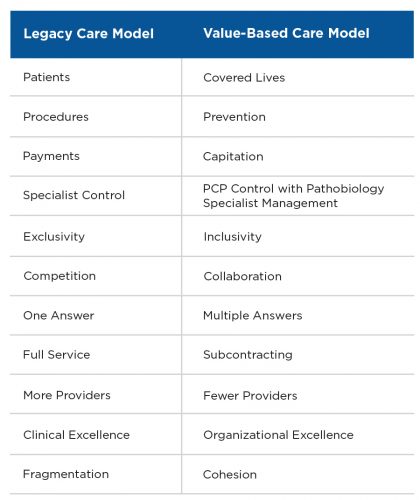
Across the United States, our health care delivery system has irreversibly changed. Some change is good. Some change may be perceived as deleterious. What is clear, however, is that providers and care delivery organizations will be increasingly challenged to perform and demonstrate value, across the spectrum, from primary care, specialty care, and subspecialty care providers.3
There is immense opportunity for entities that are prepared to embrace this needed change and assume the responsibility for managing care across the care continuum and taking the reins on managing the cost of care for patients with high needs and high costs. Physicians can and should take on the mantel of providing the proper balance of high-quality, efficient, and timely care with an eye toward maximizing the quality of life of individuals with serious illness.

Meet the Expert
Joseph Ruggio, MD, FACP, FACC, FSCAI
Founder, President and CEO, Pacific Cardiovascular Associates
President and Chief Medical Officer, Via Vitae MSO, LLC
Dr. Joseph Ruggio is a practicing Invasive, Interventional Cardiologist, and Founder and President/CEO of Pacific Cardiovascular Associates. A graduate of New York’s Albert Einstein College of Medicine, he serves as President and Chief Medical Officer of Via Vitae MSO, LLC, a strategic partnership with Fresenius Medical Care focused on cardiorenal patients, and is board certified in Internal Medicine, Cardiovascular Diseases and Interventional Cardiology.
References
Capitation of Professional Services: What We Know
by Joseph Ruggio, MD, FACP, FACC, FSCAI
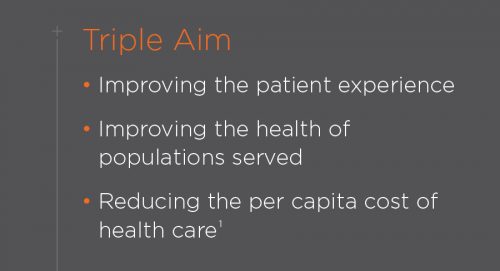
- The IHI Triple Aim. Institute for Healthcare Improvement website. http://www.ihi.org/ Engage/Initiatives/TripleAim/Pages/default.aspx. Accessed March 30, 2017.
- Cosgrove T. Value-based health care is inevitable and that’s good. Harvard Business Review, September 24, 2013. https://hbr.org/2013/09/value-based-health-care-is-inevitable-and- thats-good.
- Ward L, Powell RE, Scharf ML, Chapman A, Kavuru M. Patient centered specialty practice: defining the role of specialists in value-based health care. Chest. January 13, 2017. doi: 10.1016/j.chest.2017.01.006.



