THE CONSTELLATION OF MEASURES REFLECTED IN FIVE-STAR AND FRESENIUS KIDNEY CARE METRICS
The Centers for Medicare and Medicaid Services (CMS) assigns stars to dialysis clinics so patients can assess and compare the quality of care at various facilities. These ratings appear on the CMS’s Dialysis Facility Compare website and are based on six quality measures the agency already publishes.
This process creates a paradox: Although the CMS star rating system is an attempt to increase the number of ways to measure facility performance, are the dialysis companies’ own proprietary formulas to measure quality more reliable indicators? And further, how may the providers use the variety of public measures to guide their organization toward better patient outcomes?
What is the criteria for CMS’s Five-Star Quality Rating System for Dialysis Companies?
CMS’s Five-Star Quality Rating System is based on the dialysis centers’ standardized mortality rates, Kt/V values, hospitalizations, rates of patients with fistulas and catheters, and the standardized transfusion ratios and hypercalcemia outcomes. A significant portion of this data is acquired from the claims that hospitals and physicians submit to Medicare.
Years of intelligent analytics and predictive modeling enabled Fresenius Kidney Care (FKC) to implement a quality program that attempts to measure the observable and multidimensional components of dialysis care. While paying attention to the CMS’s Five-Star agenda, FKC focuses on furthering quality through initiatives that assess the patient experience of care within the organization and medication management, which encompasses medication reconciliation, medication efficiency, antibiotic stewardship, and the use of clinical decision support algorithms.
FKC also dedicates additional efforts to volume management, encourages hepatitis C eradication in the renal disease population, and promotes transitions of care as a key priority to improve patient safety (Figure 1).
Figure 1
The brightest constellations: Multifaceted dialysis care

Disparities in quality can occur when health care services are underused, overused, or misused.1 An example of underuse is inadequate dialysis, which can result in uremia and other related complications such as chronic inflammation and malnutrition. The overuse of health care services, on the other hand, is overtreatment with antibiotics, prescribing cascades, and polypharmacy. Beyond being costly and potentially harmful,2 health care services overuse can lead to complications in the vulnerable renal disease population. Misused services include clinical errors that may result in adverse patient outcomes and injury.
Figure 2
Constellation of measures
While CMS encourages dialysis providers to reach for the stars to facilitate improvements in the six predetermined quality measures, further advancements in care coordination in our organization may prevent or discourage underuse, overuse, or misuse of services. The FKC quality agenda supports care coordination by implementing programs such as pharmacovigilance, a hepatitis C initiative, volume management guidelines, and safe transitions of care.
When CMS implemented its rating system, the goals were to increase accountability, drive quality, improve transparency, and strengthen consumer protection which supports government’s efforts to reform our health care system. This concept can result in greater focus on disease management and enhanced patient relations. However, when the measure choice and methodology are flawed, aggregated data further amplifies any weakness in the measure and may provide inaccurate information to the consumers and damage the facility’s reputation. The star rating methodology focuses mainly on the outcomes while ignoring the underlying social determinants such as the patient mix and dialysis facility location, which could potentially cause bias.
Perceived quality based on a facility’s star rating can be very different than the actual quality of care occurring on the treatment floor. For example, a dialysis facility achieving “5-Diamond” status in patient safety and receiving top scores in patient experience of care can end up at the bottom of five-star rankings because of a handful of outlier patients with calcium results over 10.2 and an overzealous hospitalist favoring blood transfusions. Combining a few measures to rate facilities on star methodology may oversimplify the quality-of-care concept and not reflect the information most relevant to some patients and families.
Finding a Pattern Among the Stars: A Constellation
CMS acknowledges the limitations in its star rating and reminds consumers that “one star does not necessarily mean that a facility provides poor care” and that “star ratings should be used in combination with other information to choose facilities.”3
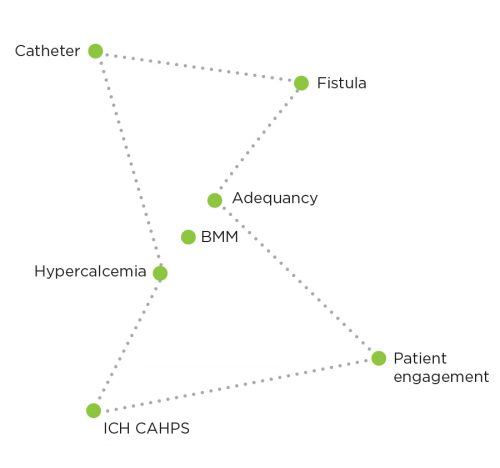
Committed to performing well in the eyes of CMS as well as our own metrics, FKC is shaping its dashboards and quality indicators around some metrics that are common to Five-Star, the Quality Incentive Program (QIP), and our Medical Office priorities, including adequacy, calcium and bone and mineral metabolism, vascular access, and patient engagement. Together, these common indicators can be thought of as a constellation of measures that show us direction and distance from our goals as we navigate to better outcomes (Figure 2).
Having established our constellation, FKC has developed a set of dashboards to help providers, managers, and executives see their position on these metrics at any given time. As an example, the Five-Star and QIP Dashboard is designed to show performance and opportunities for improvement at a patient level, in the population of patients in a clinic, and across a set of clinics in an area, region, group, or division. The various stakeholders may use the dashboard to answer questions that shape our operational priorities and what we will do next for our patients and our clinics (Figure 3).
- Clinical managers may see which patients are out of range, or view the trends and use the outcome as a catalyst to engage staff and reinforce the quality and safety goals.
- Operations and quality management teams may see how a clinic has performed across its population of patients and pinpoint which metric is the strongest or which holds the biggest opportunity for improvement.
- Senior executives gain access to information throughout the enterprise and may set priorities across a portfolio of clinics while aligning resources through a unified point of view.
In 2016, FKC quality leaders and the Medical Office partnered with operations in an effort focused on outlier management that is guided by this alignment of the stars formed by core metrics for adequacy and hypercalcemia. These efforts began paying dividends almost immediately. For example, the number of patients out of range for HD Kt/V was reduced by more than a third, from more than 3,000 patients each month during the first quarter of 2016 to less than 2,000 by the third quarter of 2016 (Figure 4).
FKC’s Information Technology and Government Reporting departments provide assistance to FKC facilities by submitting data electronically, developing business intelligence tools, sharing information about updates to CMS performance measures, and monitoring data hygiene. The Strategic Analytics department helps quality managers identify and act on opportunities to improve performance and population health. The Special Quality and Operations Team focuses on clinics that have the most opportunity for improving their performance on key star metrics.
Figure 3
As a result of the collective efforts of clinic staff and quality teams to improve our performance on the measures that form our constellation, FKC has reduced its number of clinics that have four or more of the measures out of range by more than 50 percent. This accomplishment indicates better outcomes in the eyes of external parties like CMS and, perhaps more importantly, in the eyes of patients who consult the star ratings before choosing their dialysis provider.

Summary
The renal community is still in the early stages of performance management and has not reached a consensus on what is considered a meaningful reflection of performance for dialysis facilities. Nevertheless, both the QIP and Five-Star programs—progenies of the health care reform law—brought changes that are significant and immediate. The result is a fundamental shift from volume-based to value-based payments and increased transparency that is likely to change how patients will interact with their dialysis providers.
FKC will continue its efforts to align the 5 star quality metrics into a constellation of measures that guide the organization to better outcomes. In a health care environment that prizes quality and value, attention to performance measurement and outcome improvement will be critical to the success of dialysis organizations across the system. Dialysis providers must navigate this uncharted space, organize and launch coalitions, facilitate peer-to-peer sharing, and work through the confusion to advance the frontiers of quality.
Figure 4
2016 FKC HD Kt/V The number of patients out of range for HD Kt/V was reduced by more than a third, from more than 3,000 patients each month during the first quarter of 2016 to less than 2,000 by the third quarter of 2016.
References
The Constellation of Measures Reflected in Five-Star and Fresenius Kidney Care Metrics
by Emel Hamilton & Scott Ash
- 2011 National Health Care Disparities Report. Agency for health care research and quality. October 2014. http://archive.ahrq.gov/research/findings/nhqrdr/nhdr11/index.html.
- Centers for Medicare and Medicaid Services. Dialysis facility compare & the new star ratings. 2014. https://dialysisdata.org/sites/default/files/content/new_test/Dialysis_Compare_New_ Star_Ratings.pdf.
- Ezekiel EJ. The perfect storm of overutilization. JAMA. 2008 June 18;299(23):2789- 2791. doi:10.1001/jama.299.23.2789.



