QUALITY MANAGEMENT: SOLUTIONS THAT MEET THE CHALLENGE
As the number of medically needy patients with ESRD increases, the clinic team has less time to analyze an ever-increasing amount of valuable data on patient outcomes. This quandary has increased the need to develop innovative quality management solutions. Fresenius Kidney Care is successfully implementing a multi-faceted approach that includes the application of data analysis, innovative algorithmic care and reporting with caregiver collaboration and centralized case management.
Managing clinical outcomes and pursuing improved quality and length of life for individuals afflicted with end-stage renal disease (ESRD) are essential functions of Fresenius Kidney Care (FKC). The size of the patient population, the multiplicity of their medical conditions, and the inherent complexity of dialysis treatment create operational challenges. Last year, FKC treated over 257,000 patients and, at any point in time, had over 190,000 under care. The mean age was 62, and 62 percent were diabetics. They took, on average, 10 medications per day to treat multiple comorbid conditions.
Over 26,000,000 dialysis treatments are delivered annually and generate an enormous amount of data. Every day, almost 6 gigabytes of clinical patient-specific information is added to the Fresenius Medical Care North America (FMCNA) Knowledge Center. As the ESRD population has grown, the supply of nephrologists has not kept pace, resulting in a higher patient load per doctor. Dialysis clinic staff provide more sophisticated care to sicker patients, which can jeopardize the time available for thoughtful and reflective analysis of outcomes. The combination of more data and more medically needy patients increases the need for organized quality management solutions.
To address this challenging situation, FKC has adopted a series of innovations in care management and technology to assist clinicians in the pursuit of continuous quality improvement. These include:
- Algorithms for care
- Outcome reporting solutions that are relevant, transparent, and accessible
- Information systems that provide critical clinical information in real time during treatment
- IT solutions that support the performance of formal quality assessment and improvement activities
- Focused interventions to identify and manage patients with specific needs
- Staff education on continuous quality improvement
Algorithms
Algorithms are distinct care paths based on best practice evidence, using data to guide decision making, medication adjustment, and clinical interventions in an orderly manner. The development of clinical care pathways requires a balance between efficient decision making and adjustment of treatment, and individualization of care. Algorithms at FKC are developed analyzing published scientific literature in collaboration with expert medical opinion provided by physicians on the Pharmacy and Therapeutics Committee and the Corporate and Divisional Medical Advisory Boards. All algorithms are treated as physician orders. They are made available as a resource but ultimately are used at the doctor’s discretion. These tools are created either as automated programs that intake data and respond with recommended changes in therapy, or as documents (paper and electronic) that are available on demand to guide treatment.
As of Q1 2018, algorithms available at FKC are:
- Anemia management with Mircera, Aranesp, Epogen, and iron
- Evaluation of ESA hyporesponsiveness
- Bone and mineral metabolism (vitamin D analogues, calcimimetics)
- Hypercalcemia
- Fluid management
- Crit-Line operation
- Dialysis adequacy
- Transition from venous catheter to permanent vascular access
- Evaluation and treatment of hepatitis C
These algorithms provide guidance for both individual physicians and focused intervention groups at FKC.
Identification of Goals and Measurement of Quality Status
Improvement requires a clear understanding of current performance and trends as well as a clear definition of goals. The ESRD space abounds with clinical measures, including the CMS Five Star and QIP programs. The 2017 FKC Medical Office Quality Agenda described five areas of performance for all patients in relation to the patient experience.
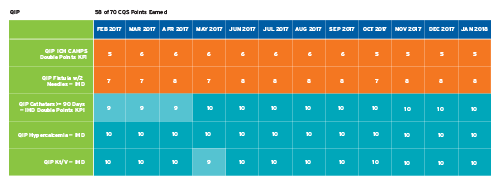
To better organize, measure, and communicate progress toward these goals in 2017, FKC introduced a new Clinical Quality Status Report (CQS). CQS is structured in three sections: QIP, Clinical Outcomes, and Clinical Processes. Each section is composed of multiple topics. In the QIP section, performance is reported in relation to CMS thresholds. The other two sections are intended to highlight a broader menu of impactful measures and the behaviors necessary to drive improvement. Clinics are ranked, and points are assigned by relative percentile standing for performance to a standard. Reporting is delivered electronically, with a useful color scheme, panels of related information, and a hierarchical structure featuring drill-down functionality from company level to division, region, area, clinic, and patient details (Figure 1).
Figure 1 | “Heat map” of CQS outcomes

Management of Data for Quality Improvement Activities
Aggregated clinical data must be organized, trended, and evaluated to be of value. The monthly Quality Assessment and Performance Improvement meeting at each clinic is the venue for these activities. Historically, many hours were spent assembling the data for these meetings. In 2017, the Electronic Quality Improvement Program (eQUIP) was launched. This application pulls data from the clinical systems and CQS, organizes it, and creates comparisons to target performance. Trends are analyzed, and opportunities for change are identified. As with the algorithms, certain standard interventions are suggested from a catalog of activities, but the interdisciplinary team can create and document individual projects as well. Subsequent achievement due to these plans is tracked, creating the opportunity to review them as needed.
Critical Information at the Right Time
Changes in therapy should be delivered in a timely manner. The greatest opportunities to appropriately make such changes is when the patient is in the clinic and when the latest information is freshly available. In 2017, the FKC Chairside Information System was updated to present detailed and relevant information about patients’ volume status. By highlighting deviations from estimated dry weight (EDW), blood pressure extremes (Figure 2), and physical findings of fluid overload, the treating technician and nurse are prompted to discuss appropriate changes with the nephrologist. An electronic version of the volume algorithm is presented and can direct necessary prescription adjustments. Other new process alerts presented at chairside include positive blood cultures, new antibiotic sensitivities, conversion of hepatitis B status, inadequate Kt/V, and hypercalcemia.
Figure 2 | Chairside Treatment Summary screen

Management of Special Populations
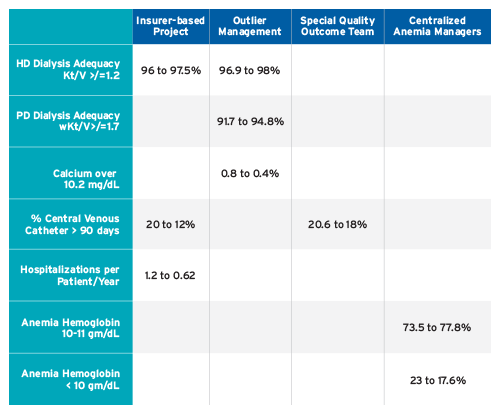
As quality projects progress, it is not unusual to find locations with either unique challenges or small groups of patients who fail to improve with the usual interventions. Such situations were characterized as “outliers” in FMCNA’s 2017 Annual Medical Quality Report. In four projects, case managers in FKC Quality and Value Based Services focused on patients needing special attention. These projects were QIP outlier management for hypercalcemia and dialysis adequacy, anemia management to assist in cases of recalcitrant anemia, special quality outcomes team for clinics with multiple areas of underperformance, and a quality performance-based contract for a major commercial insurer.
The following elements contributed to the success of these initiatives:
- Informatics structured to deliver timely reports to identify outliers and provide critical clinical information to facilitate root-cause analysis of suboptimal outcomes
- Dedicated teams of RN case managers
- Utilization of algorithms established by the Corporate Medical Advisory Board, evidence-based best practices, and consistent policies and procedures
- Collaboration between the intervention teams and the interdisciplinary team at the clinic
- Ongoing analysis of outcomes to trend responses to interventions and guide modifications
Demonstrated Success
Although operating with different patient populations and for differing durations of intervention, each group employing the methodology detailed above experienced success, as demonstrated by:
A Culture of Accountability
In 2017, the FKC Quality Department launched the Quality Collaborative Model. This effort was intended to transparently demonstrate quality performance and establish accountability at all levels of the operational organization. Each level—Corporate, Group, Region, Area, and Clinic—was assigned responsibility for performance of their quality activities, supervision of the actions at their facility, and reporting upward through the organization. Monthly Quality Flash Reports established by FKC are analogous to the corporate financial meetings and are designed to review progress, celebrate successes, and explore challenges.
Conclusion
The challenge of quality management in FKC’s large, diverse, and complex patient population is being met with the application of data analysis, innovative algorithmic care, collaboration with caregivers, timely reporting of outcomes, centralized case management, and a culture of accountability. Refinements in these areas will contribute to FKC success in continuous quality improvement.
Meet Our Expert
Jeffrey Hymes, MD
Chief Medical Officer, Fresenius Kidney Care
Jeffrey Hymes, chairman of the FKC Pharmacy and Therapeutics Committee, is board certified in internal medicine, nephrology, and critical care. He co-founded REN Corporation in 1986 and National Nephrology Associates (NNA) in 1998, and served as NNA’s president and chief medical officer from 1998 to 2004. He is a graduate of Yale College and the Albert Einstein College of Medicine. He completed his medical internship and residency at Yale New Haven Medical Center and received subspecialty training in nephrology at Boston University.



